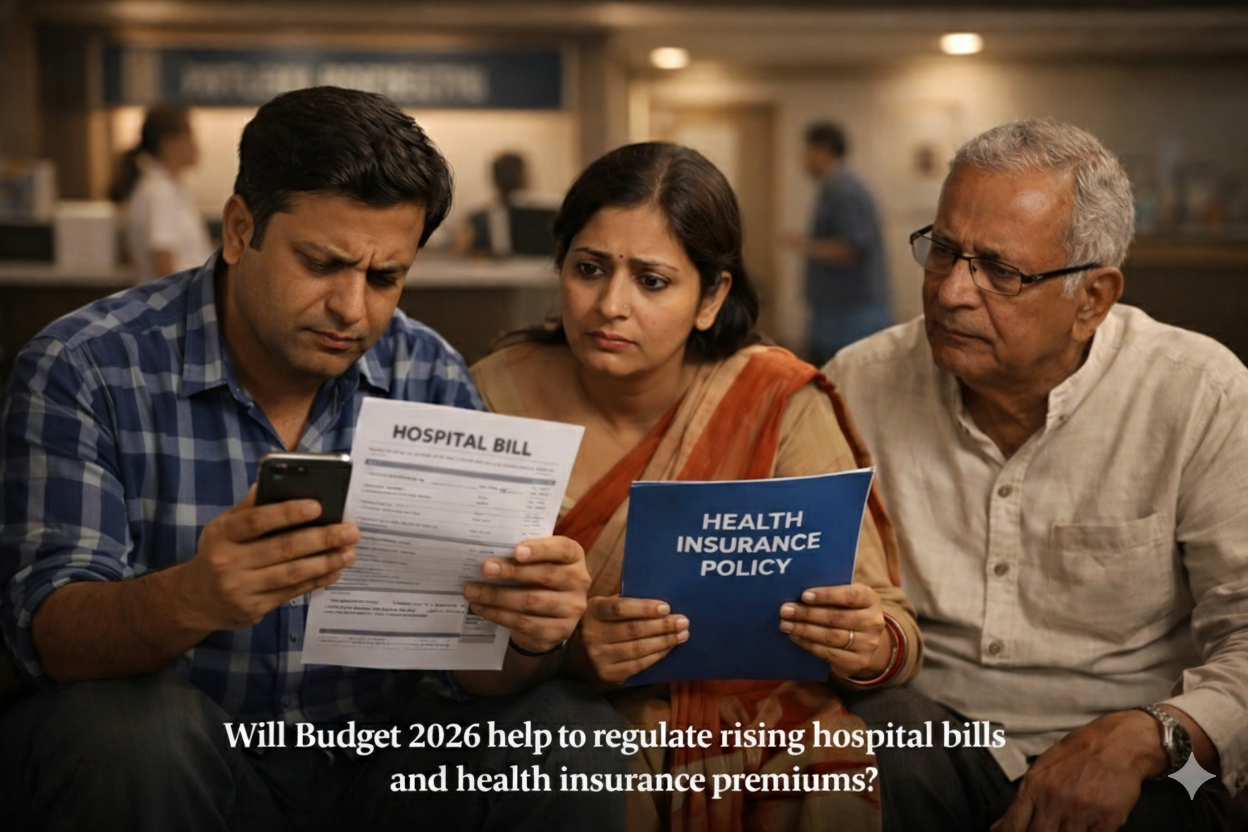
On a particularly cool June night in Meerut, Uttar Pradesh, 60-year-old Ashish Jha found himself reeling from severe chest pain. A visit to a nearby hospital didn’t help. His insurance policy, meant to be a lifeline, was unable to provide cashless treatment for his heart surgery as the hospital lacked the facilities for cashless claims settlement.
Cashless treatment, where the health insurer settles the patient’s bills directly with the hospital, has been a pet project of the Insurance Regulatory and Development Authority of India (Irdai). It has raised the bar further, mandating that all cashless claims be processed within three hours of the receipt of discharge authorisation and has asked insurers to put necessary systems in place by July 31. But as the example above illustrates, the initiative faces significant hurdles. Per the latest Irdai report, 42% of the 23.36 million claims in 2023 were settled through reimbursements.
Recently, the Irdai introduced a series of reforms to enhance policyholders’ access to and benefits from health insurance. These changes specifically address concerns such as quick cashless treatment everywhere, pre-existing disease coverage, and inclusion of senior citizens.
The question now is, will these reforms lead to a smoother experience for policyholders, or will they be presented with more challenges?